|
Introduction
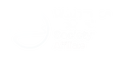
The pelvis is an integral part of the human skeletal system and contains some of the largest bones in the body. Structurally, it connects the lumbar spine to the lower extremities and carries and supports the abdominal organs. Its right and left sides (coaxe) are formed by the fused bones of the ilium, ischium, and pubis; an outside socket on each coxa (the acetabulum) holds the femoral head. Internal ligaments connect the sacrum to both sides in the back at the sacroiliac joint and to one another in the front at the symphysis pubis to form a circle. When intact, the combination of bones and ligaments create an amazingly strong structure capable of withstanding a significant amount of pressure. That said, fractures and ligament damage can occur. While most pelvic injuries are minor, a few can cause severe internal hemorrhage and death. Fractures of the two rings (rami) at the bottom of the pelvis and fractures of the iliac wing, although painful, are rarely serious. On the other hand, fractures of the sacrum or ilium, separation of the symphysis pubis, or tears to major pelvic ligaments that cause the pelvis to open like a book, shear vertically, or compress inward may cause massive internal bleeding and are usually life-threatening. Most serious pelvic injuries are caused by high energy events: falls from a height, motor vehicle accidents, and crush injuries. While torn ligaments can bleed profusely, the majority of bleeding associated with pelvic injuries is typically venous bleeding directly from the fracture site. Arterial bleeding is rare and usually leads rapidly to death from volume shock. Blood accumulates in the retroperitoneal space (which is capable of holding up to four liters) and if the pressure is great enough, may also track into the abdomen; genitourinary and gastrointestinal damage often accompany seriour pelvic injuries. Internal volume and bleeding increase with open-book injuries as the coxae splay backward. Click on an image to enlarge.
0 Comments
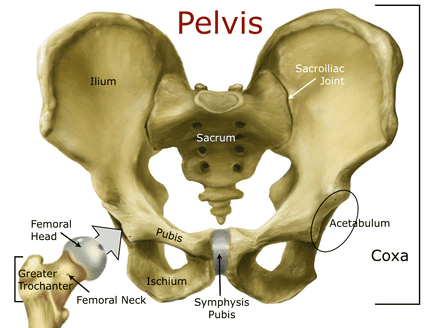
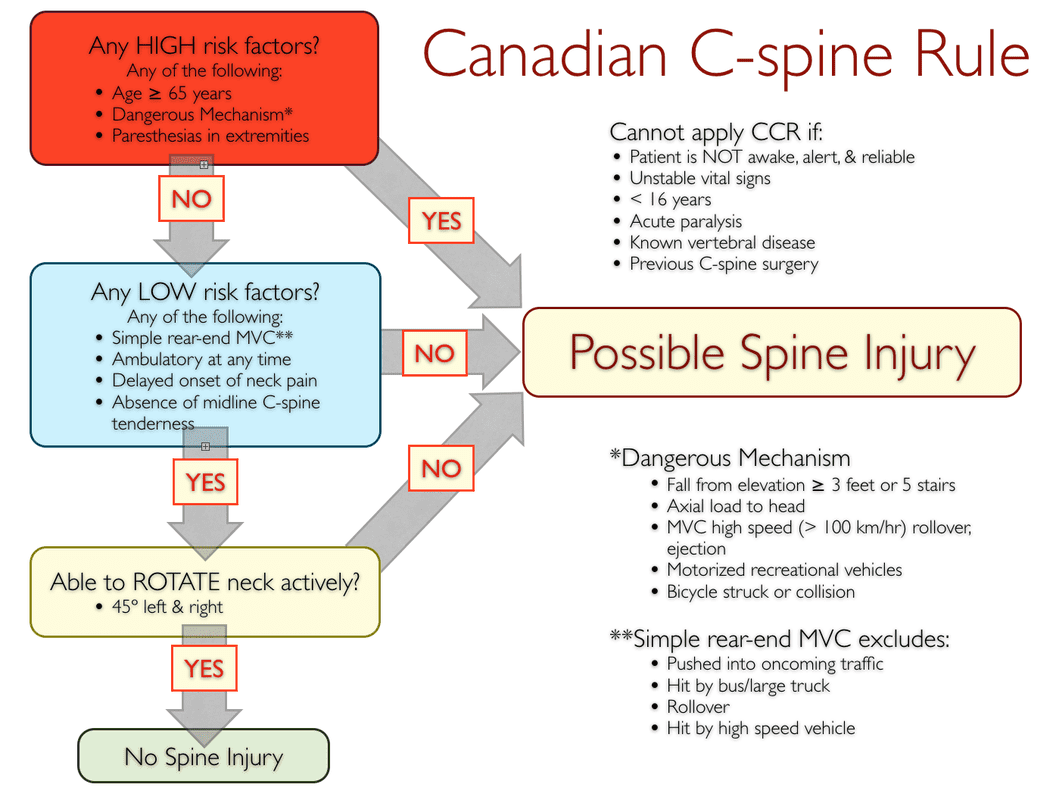
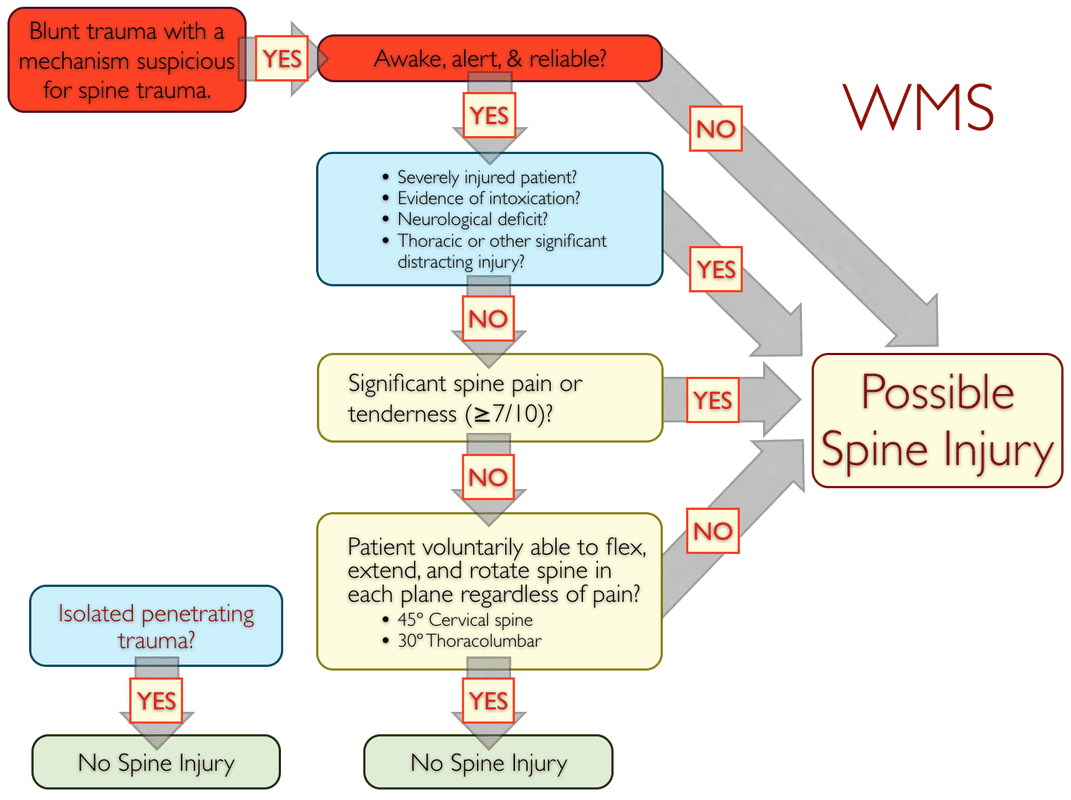
There are five commonly used protocols for ruling out possible spine injuries in the field: the Canadian C-spine Rule (CCR), the National Emergency X-Radiography Utilization Study (NEXUS) low-risk criteria (NEXUS), the modified Nexus criteria, the State of Maine criteria (also based on the NEXUS criteria), and the Wilderness Medical Society (WMS) algorithm (a combination of the CCR and NEXUS). All are backed by solid research, in common use, and summarized below; click on an image to enlarge it. Here's a quick summary of the differences: The CCR primarily focuses on ruling out the potential for a cervical spine injury by looking closely at the mechanism of injury. The NEXUS, modified NEXUS, State of Maine protocols, and the WMS guidelines assume a spine injury and focus on ruling it out via signs and symptoms. The difference between the NEXUS and modified NEXUS is the NEXUS study focuses on the cervical spine while the modified NEXUS has been adapted for the entire spine. The original NEXUS criteria does not include assessing the patient's spine pain, the modified NEXUS does and, as such, is more conservative than the NEXUS. The State of Maine criteria adds paraspinal tenderness to the mix, while the WMS guideline is a combination of the CCR and modified NEXUS. The term focused spine assessment (FSA) is somewhat generic and may refer to any of the above protocols.
For over four decades and with little or no data to back it up, EMS fully immobilized all patients involved in major traumatic incidents in order to prevent neurological damage from a potential spine injury. The premise underlying this practice was that a major traumatic event could injure the patient's spine and subsequent spinal movement would result in a cord injury, and full external spinal immobilization would prevent said movement. This precept is seen as false and spine management in both urban and wilderness environments has changed—or is in the process of changing—accordingly. Read on to see how and why this transformation has taken place...and what the current spine management guidelines are for wilderness and remote locations.
Ankle injuries are, unfortunately, all to common on outdoor trips. Even though both stable and unstable ankle injuries cause soft tissue damage and swelling, field assessment is simple and based primarily on the patient's range of motion (ROM) and whether or not they are able to stand and bear weight shortly after the event. If their ROM is intact and they are able to bear weight, the injury is stable; if not, the injury is unstable.
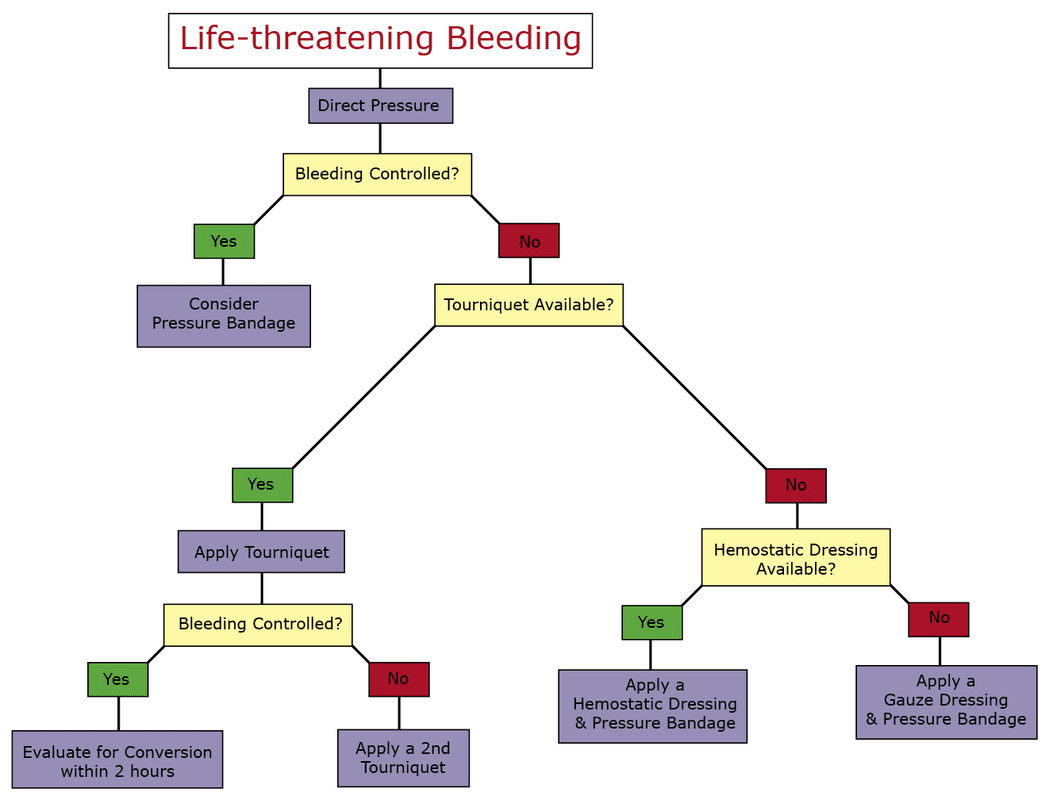
The vast majority of stable ankle injuries in the outdoors result from rolling the ankle laterally (to the outside) while hiking or running on an uneven surface. If the patient has no obvious deformity, tenderness slightly in front of and below the lateral malleolus (ankle bone on the ouside of the patient's leg), and can bear weight shortly after the event they probably have an uncomplicated lateral ankle sprain (sprain = ligament damage). If the ankle rolls inward (rare) the medial ligament complex may be damaged. Again, if the patient has no obvious deformity, presents with tenderness slightly below the medial malleolus (ankle bone on the inside of the patient's leg), and can bear weight shortly after the event, in all likelihood they have an uncomplicated medial ankle sprain. In uncomplicated ankle sprains, swelling can be prevented with compression around both malleoli (ankle bones), elevation of the injured ankle higher than the heart, cold water baths, and pain-free ROM and light strengthening exercises 2-3 times a day. Commercial compression donuts are super lightweight and come coated with a waterproof skin adhesive; simply peel off the backing and attach. Ideally, the patient should avoid extended walking on the injured ankle for 2-5 days. If the patient must walk during this time, you will need to support their ankle and significantly reduce their pack weight. Whether a patient requires an evacuation for an ankle sprain depends of the severity of the injury, the type of activity (backpacking, cycling, canoeing, etc.), and the difficulty of the terrain they can be expected to traverse. The first set of photos below show how to improvise a walking splint using a padded aluminum splint and foam donuts to deliver focal compression to the soft tissue surrounding the malleoli in order to prevent excessive swelling and promote rapid recovery in uncomplicated ankle medial or lateral ankle sprains. The second set show how to improvise a splint for an unstable ankle injury and adapt an expedition backpack to safely evacuate the patient. While common in military and para-military tactical situations, terrorist attacks, and explosions, and somewhat common in motor vehicle and farm machinery accidents, life-threatening bleeding is rare in a recreational wilderness environment. Chainsaws, ice-climbing tools, tree stubs, motorboat props, etc. can elicit significant injuries. Rescuers should assess all trauma patients for external bleeding that, if not immediately controlled, may rapidly lead to volume shock and death. Most life-threatening bleeding is arterial; however, severe venous bleeding is possible. Hemophiliacs and patients taking anticoagulant medications may be at extreme risk from even small lacerations. Closely examine all trauma patients for significant bleeding. Remove or cut clothing and visually inspect the wound. If necessary, wipe away excess blood. Feel for blood in areas that are difficult to see. Arterial blood is bright red and spurts out of a wound in time with the patient's pulse; in contrast, venous blood is darker and while it does not spurt, blood loss can be heavy. Severe, life-threatening bleeding, while extremely rare in a wilderness setting, must be controlled quickly as death from exsanguination can occur within minutes. The primary tools are well-aimed direct pressure, pressure bandages, commercial tourniquets, and hemostatic dressings; pressure points and elevation are ineffective. Well-aimed direct pressure is first step in controlling severe bleeding and, if successful, often followed by the application of a pressure bandage. Guidelines for Applying Direct Pressure
Guidelines for Applying a Pressure Bandage
Extremity Tourniquets The successful use of commercial extremity tourniquets by the military over the past decade has saved countless lives. With the proper training, commercial tourniquets—CAT, SOF-TT, SOF-TT wide, and SAM XT—are effective and safe to use in a wilderness environment. Two large military studies conducted in Iraq show respectively a 90% and 96% survival rate when commercial tourniquets were applied before the onset of volume shock, 4% and 10% survival when applied after the onset of volume shock, and 0% survival rate when not applied but needed. These studies clearly indicate that properly applied commercial tourniquets are both safe and effective as a first line treatment for life-threatening bleeding on the extremities. Does this mean that you should carry a commercial tourniquet in your first aid kit while hiking, skiing, paddling, climbing, etc.? Probably not, but it is worthy of consideration. Remember, severe extremity bleeding, while common on a battlefield or in a tactical situation, is extremely rare in an expedition setting. Tourniquets are more likely to be needed when machines—chain saws, chippers, wood splitters, farm machinery, etc.—are used in remote setting or when responding to a serious vehicle accident. Given their relatively small size, lightweight construction, and low cost, it makes sense to carry a commercial tourniquet if you are a member of a paramilitary group (police, warden, ranger, etc.), working with farm or logging equipment, or in your vehicle first aid kit, not so much in your expedition kit. It’s important to note that improvised tourniquets have been shown to be generally ineffective due to the time it takes to locate the necessary supplies and apply it, and the skill required to engineer it. A venous tourniquet—one that shuts down the venous system but not the arterial system—is not effective and can reduce core blood volume and lead to a compartment syndrome. Most rescuers are surprised at the amount of force required to block arterial flow to the extremity. If you think you might need an improvised tourniquet, carry a commercial tourniquet instead. If you choose to carry a commercial tourniquet, you need to practice and master its use before you rely on it in a field situation. Application Guidelines for Commercial Extremity Tourniquets
Once a tourniquet is in place, evaluate it in a controlled situation within two hours. Tourniquets left in place for greater than six hours may cause significant tissue damage. Do not attempt conversion if the patient has an unstable critical system problem, bleeding disorder, or taking Rx blood thinners. Conversion Guidelines for Commercial Extremity Tourniquets
Hemostatic Dressings Hemostatic dressings are used in conjunction with pressure bandages when a tourniquet is unavailable or or inappropriate, as in junctional or truncal bleeding). As with tourniquet use, the first step is to apply direct pressure to the site. While many of the first generation hemostatic agents had problems and are no longer commercially available, third generation dressings have few issues and made with chitosan or kaolin. Dressings made with chitosan—Celox Gauze, ChitoGauze, and ChitoSAM—react with blood to form a localized clot independent of the normal clotting cascade. Dressings made with kaolin—Combat Gauze—activate the intrinsic coagulation pathway. Unlike kaolin, that remains in the body, chitosan is naturally broken down by bodily enzymes and cleared. Since ChitoSAM gauze is made from 100% chitosan (rather than chitosan impregnated gauze) and can be left in the wound longer than other hemostatic dressings, it is more suitable for use in remote settings when evacuation is delayed. Application Guidelines for Hemostatic & Gauze Dressings
If you think a wound is bleeding severely, treat it as if it is and follow the steps outlined in the following algorithm: Looking for a reliable field reference? Consider consider purchasing one of our print or digital handbooks; our digital handbook apps are available in English, Spanish, and Japanese. Updates are free for life. A digital SOAP note app is also available.
Padded Aluminum Splints may be purchased at our online store and fit into the outside zippered pockets on our Guide and Expedition first aid packs.
|
Categories
All
Our public YouTube channel has educational and reference videos for many of the skills taught during our courses. Check it out!
|



 RSS Feed
RSS Feed