|
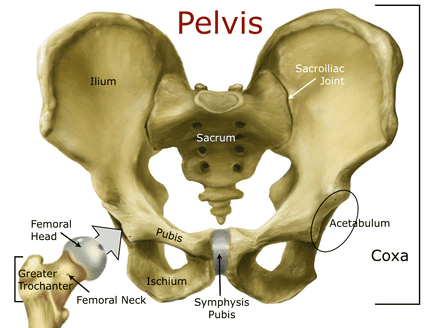
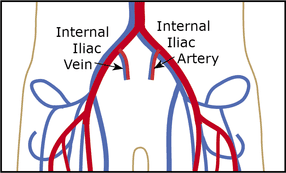
Introduction The pelvis is an integral part of the human skeletal system and contains some of the largest bones in the body. Structurally, it connects the lumbar spine to the lower extremities and carries and supports the abdominal organs. Its right and left sides (coaxe) are formed by the fused bones of the ilium, ischium, and pubis; an outside socket on each coxa (the acetabulum) holds the femoral head. Internal ligaments connect the sacrum to both sides in the back at the sacroiliac joint and to one another in the front at the symphysis pubis to form a circle. When intact, the combination of bones and ligaments create an amazingly strong structure capable of withstanding a significant amount of pressure. That said, fractures and ligament damage can occur. While most pelvic injuries are minor, a few can cause severe internal hemorrhage and death. Fractures of the two rings (rami) at the bottom of the pelvis and fractures of the iliac wing, although painful, are rarely serious. On the other hand, fractures of the sacrum or ilium, separation of the symphysis pubis, or tears to major pelvic ligaments that cause the pelvis to open like a book, shear vertically, or compress inward may cause massive internal bleeding and are usually life-threatening. Most serious pelvic injuries are caused by high energy events: falls from a height, motor vehicle accidents, and crush injuries. While torn ligaments can bleed profusely, the majority of bleeding associated with pelvic injuries is typically venous bleeding directly from the fracture site. Arterial bleeding is rare and usually leads rapidly to death from volume shock. Blood accumulates in the retroperitoneal space (which is capable of holding up to four liters) and if the pressure is great enough, may also track into the abdomen; genitourinary and gastrointestinal damage often accompany seriour pelvic injuries. Internal volume and bleeding increase with open-book injuries as the coxae splay backward. Click on an image to enlarge. It's worth noting that the force required to cause a serious pelvic injury makes associated traumatic injuries common: over 90% of patient's with pelvic ring injuries also have head or chest injuries. The majority of these multi-trauma patients will die if their injuries occur in a remote setting where Advanced Life Support and rapid transport are unavailable. For those that survive, recovery is a long-term process and fraught with complications.  Assessment Assessment of pelvic injuries begins with a close examination of the MOI; low energy events are unlikely to produce serious injuries. In the backcountry, falls from a height, high speed bicycle and ski/snowboard crashes, and avalanche are often mechanisms. Significant pelvic injuries are accompanied by severe pain and patients often faint (secondary to a parasympathetic autonomic stress response). It's vital to avoid extraneous pelvic movement during the physical exam: rocking the patient's pelvis or rolling them onto their side may displace fractured bones, disrupt clotting, and increase local both damage and bleeding. Closely monitor the patient's pulse, blood pressure (if possible), and level of consciousness for the classic clinical pattern of internal bleeding and volume shock: Initially (early volume shock), as the patient bleeds internally, they are awake with increasing levels of anxiety with:
As bleeding continues (late volume shock), the patient will become voice responsive, pain responsive, and eventually unresponsive with:
Things to consider during your physical exam:
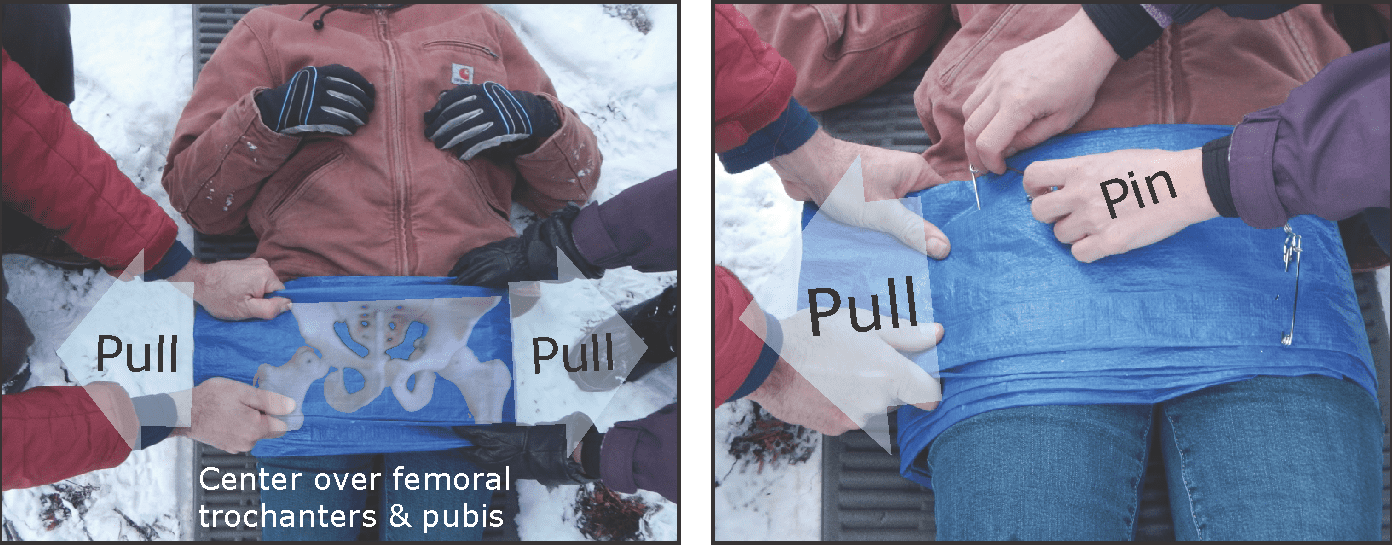
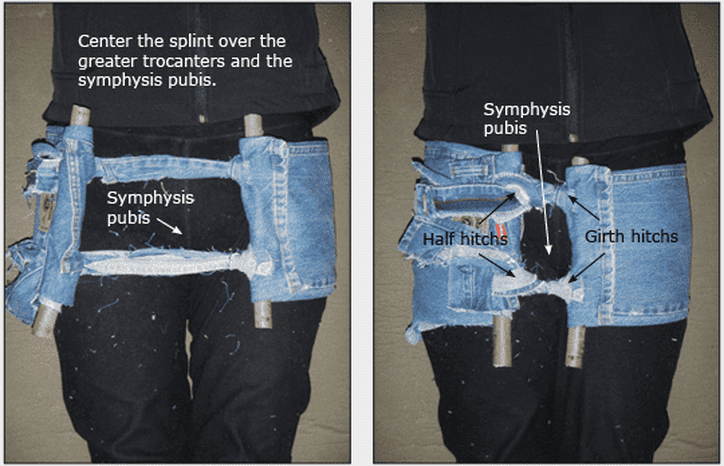
Treatment Pre-hospital treatment focuses on external stabilization of the pelvic ring to reduce internal volume, bleeding, and pain. Rapid litter transport to a major hospital for definitive evaluation and surgery is essential for survival. Two methods of improvising an effective pelvic splint are show below. Focus on understanding the structural concepts; the materials you use will vary depending on what is available. Method 1: Pinning
Method 2: Pelvic Corset 
Want more information on this and other wilderness medicine topics? Take one of our wilderness medicine courses. Guides and expedition leaders should consider taking our Wilderness First Responder course. Looking for a reliable field reference? Find this information difficult to remember? Looking for a reliable field reference? Consider consider purchasing one of our print or digital handbooks; our digital handbook apps are available in English, Spanish, and Japanese. Updates are free for life. A digital SOAP note app is also available.
0 Comments
Your comment will be posted after it is approved.
Leave a Reply. |
Categories
All
Our public YouTube channel has educational and reference videos for many of the skills taught during our courses. Check it out!
|


 RSS Feed
RSS Feed
