|
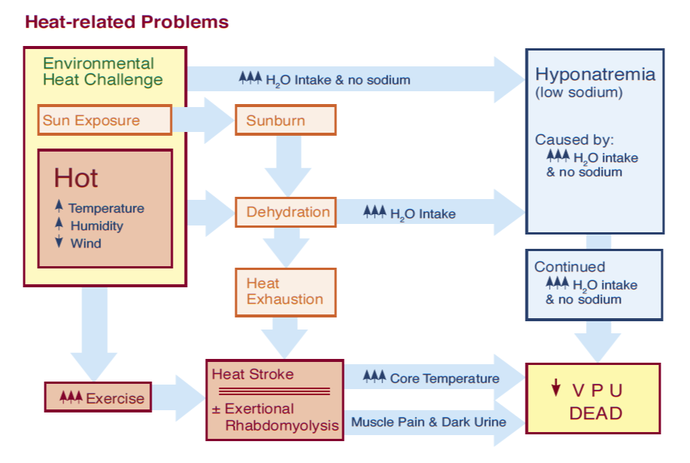
Introduction Heat is part of summer; some people love it...and others, not so much. Regardless of which camp you reside in, excessive heat, typically combined with exercise, can cause a number of potentially fatal, and certainly uncomfortable, heat and heat-related problems (e.g., dehydration, heat exhaustion, heat stroke, exertional rhabodomyolysis, and exercise-associated–exertional–hyponatremia; refer to the graphic below to see the relationship between the major heat related problems). Prevention and proper hydration is key to avoiding all heat-related illnesses, and the cornerstone of prevention is to allow your body enough time to acclimatize to a new heat challenge. With that said, the drugs listed below can predispose outdoor adventurers to a variety of heat illnesses and heat-related problems. Check to see if your friends, clients, or students are taking any of them before venturing into the outdoors this summer when it's hot outside. (A printed drug guide, app, or website will help you understand the side effects, contraindications, and administration guidelines for most drugs.) If you find that they are taking a drug that predisposes them to a heat illness:
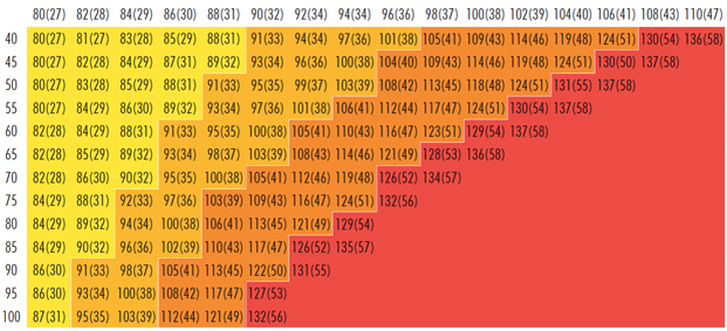
The National Weather Service (NWS) heat index values in the above chart are for shaded, light-wind conditions. Exposure to full sunlight can increase heat index values by up to 15° F; and, strong winds, particularly with very hot, dry air, can be extremely hazardous Anticholinergics Anticholinergic drugs block the transmission of the neurotransmitter acetylcholine in the central and peripheral nervous system responsible for the autonomic control of the smooth muscles primarily in the gastrointestinal (GI) tract, the genitourinary tract, and the lungs. They are used to treat:
Antihistamines Antihistamines block histamine receptor sites in mast cells and basophils, smooth muscle, the lining of lymph and blood vessels, and histamine-releasing neurons in the brain. There are two subcategories of antihistamines: H1 and H2; both are used to treat allergies. H2 antihistamines, because they bind to histamine receptors in the gut, are also used to treat peptic ulcers and acid reflux and H1 antihistamines, because they cross the blood-brain barrier and bind to histamine receptors in the hypothalamus, may be used to treat insomnia in adults and motion sickness. Similar to anticholinergic drugs, antihistamines inhibit sweating and predispose people to both heat exhaustion and heat stroke. Opioids Opioids—including their semi-synthetic and synthetic derivatives—are used to manage both acute and, to a lesser extent, chronic pain; strong opioids are highly addictive. Codeine, a weak opioid, is commonly used in over-the-counter (OTC) pain medications and cough suppressants. Loperamide, an opioid that cannot cross the blood-brain barrier acts on the large intestine to suppress diarrhea. All opioids decrease blood flow to the skin and predispose people to heat stroke. Pseudoephedrine Pseudoephedrine is a stimulant that acts on the smooth muscle lining the blood vessels and bronchi causing them to constrict; it is used to treat sinus and nasal congestion and promote drainage of the sinuses and the Eustachian tubes. Because it's a vasoconstrictor, pseudoephedrine decreases blood flow to the skin and predisposes people to heat exhaustion and heat stroke. Diuretics Prescription diuretics are first-line drugs used to treat high blood pressure. Along with caffeine, prescription diuretics promote dehydration via excessive urination and, through that route, predispose people to heat exhaustion, heat stroke, and—because they deplete the body of sodium—hyponatremia. Selective Serotonin Reuptake Inhibitors (SSRIs) SSRIs are a class of drugs primarily used to treat depression and anxiety disorders but may also be used to treat post traumatic stress disorders (PTSD). The exact therapeutic mechanism is unknown and the side effects of SSRIs may outweigh their benefit. All SSRIs can cause dehydration, which, in turn, can lead to more serious heat illnesses. Ibuprofen & Naproxen Both ibuprofen & naproxen belong to a family of drugs called non-steroidal anti-inflammatory drugs (NSAID) that are commonly carried in first aid kits to treat pain or reduce a fever. While neither drug predisposes people to a heat illness, CAUTION is advised as they can cause kidney damage in the presence of dehydration. Antipsychotics Antipsychotics block receptor sites in the brain's dopamine pathways and are used to treat schizophrenia and bipolar disorders, and combined with antidepressants to treat depression in the short term. Unfortunately, they can inhibit the body’s ability to regulate temperature and predispose people to heat stroke. Beta Blockers Beta receptors are found in the smooth muscle cells of arteries, bronchi, kidneys, and the heart. When stimulated by epinephrine and other stress hormones, they cause a sympathetic stress response that, among other things, increases heart rate and blood pressure. Beta blockers weaken the stress response and are primarily used to manage abnormal heart rhythms and prevent a second heart attack. (They may also be used to treat high blood pressure but are not as effective as diuretics.) They reduce blood flow to the skin and and predispose people to heat stroke. Calcium Channel Blockers Calcium channel blockers disrupt the movement of calcium through cell membranes and are used to treat high blood pressure. They help increase the elasticity of the wall of large blood vessels allowing them to stretch and expand. In this way they also reduce chest pain caused by angina pectoris. They are more effective than beta blockers but have more side effects. Similar to beta blockers, they also reduce blood flow to the skin and predispose people to heat stroke. Ephedrine, Amphetamines, & Cocaine Ephedrine, amphetamines, and cocaine are central nervous system stimulants. Ephedrine is used as a stimulant, appetite suppressant (currently banned in the United States), concentration aid, and decongestant; it works by increasing the activity of norepinephrine. Amphetamines are used to treat attention deficit hyperactivity disorder (ADHD) and narcolepsy. Cocaine is made from the leaves of the coca shrub with no current medicinal use; it is primarily used as a recreational drug...as are many amphetamines. Ephedrine, amphetamines, and cocaine increase internal body temperature, constrict blood vessels, and predispose people to heat exhaustion and heat stroke. Tricyclic Antidepressants Tricyclic Antidepressants (TCAs), as the name implies, are primarily used in the treatment of mood disorders; they are also used to treat chronic neuropathic pain and as migraine prophylaxis (but will not treat a migraine attack). TCAs also decrease sweating and inhibit the body’s ability to regulate temperature and predispose people to heat exhaustion and heat stroke. ACE Inhibitors ACE inhibitors are primarily used to treat heart and kidney problems. They block the production of enzymes that cause vasoconstriction and permit blood vessels to relax (dilate) reducing both blood and kidney pressure. ACE inhibitors may cause increased sweating in some patients, which may quickly lead to dehydration in a heat challenge, and by that route predispose people to heat exhaustion and heat stroke. Lithium Lithium is a mood stabilizer used to treat bipolar disorders and is primarily cleared via urine. While lithium does not predispose people to any heat illness, if a client taking lithium loses a lot of fluid quickly through sweating—which, depending on the individual can easily occur in a moderate or severe heat challenge—their lithium level may quickly rise to toxic levels.
Looking for a reliable field reference? Consider consider purchasing one of our print or digital handbooks; our digital handbook apps are available in English, Spanish, and Japanese. Updates are free for life. A digital SOAP note app is also available.
0 Comments
Human health is linked to the health of the environment, including its plants and animals (yes, insects are classified as animals: Kingdom Animalia > phylum Arthropoda). Infectious diseases in humans are caused by viruses, bacteria, parasites, or fungi, and transmission is via one of four routes:
Looking for a reliable field reference? Consider consider purchasing one of our print or digital handbooks; our digital handbook apps are available in English, Spanish, and Japanese. Updates are free for life. A digital SOAP note app is also available.
Contrary to how it is often depicted in movies, the act of drowning often goes unnoticed. There appear to be three separate actions or body positions people adopt when confronted with the possibility of drowning. Depending on their swimming ability, injuries, or illnesses, some will progress through all three of these stages, while others will not.
In a drowning, the victim is submerged under or immersed in water and requires rescue or assistance; not all drowning victims are unresponsive during their rescue and upon recovery, some are awake, voice responsive, or pain responsive. Drowning is a process with three possible outcomes: 1. Death, 2. survival with brain damage, and 3. survival without brain damage. In rare cases, primarily associated with cold water and young children, a few pulseless and apneic victims may also have a complete recovery if rescued within 30-90 minutes—depending on water temperature—and CPR started immediately. These fortunate few will have experienced an immediate shell/core response from core hypothermia or a phenomenon known as the "Mammalian Diving Response" or MDR. Many, but not all, drowning victims will quickly become unresponsive due to a systemic loss of oxygen and minutes later their heart will stop; in most cases, after roughly five more minutes they will suffer permanent brain damage. If not rescued, all unresponsive drowning victims will die. If rescued, the unresponsive patient who still has a pulse (but is not breathing) has a reasonable chance for recovery if rescue breathing is begun immediately. A patient who has no pulse and no respirations may, with immediate CPR, also recover completely, however, mortality is high. Given the potential for core hypothermia or an MDR, start CPR on all pulseless and apneic drowning victims who have been submerged for less than 30 minutes in water warmer than 43ºF (6ºC) or less than 90 minutes in colder water. If a recovery occurs during CPR, it will usually happen within the first few minutes. If pulse and respirations are not forthcoming, continue resuscitation efforts for a full 30 minutes. Click to read an article on cold water immersion. Most drowning victims aspirate very little water because their epiglottis closes and they swallow; the water, sometimes a LOT of water, enters their stomach. The majority of non-fatal drowning patients asperate less than 30 ml (1 oz) of water while fatal drowning patients aspirate 1-2 ml of water per kg of body weight (as found during autopsy). The aspirated water is absorbed into the microvascular bed surrounding the alveoli where it may wash out leading to alveolar collapse and cause an inflammatory response that leads to pulmonary edema (PE). In most cases, the S/Sx of PE will appear within 2-3 hours and non-fatal drowning patients should be monitored for 4-6 hours. Listening with a stethoscope—and occasionally with an ear to the patient's bare chest—will reveal rales, crackling noises that indicate fluid is accumulating in the patient's lungs. Foam in the patient's upper airway—or issuing from their mouth or nose—is the result of plasma (PE) mixing with the displaced surfactant. Decreased water quality increases the likelihood of pulmonary edema and subsequent respiratory infections. Fleas, mosquitoes, lice, assassin bugs, sand flies, chiggers, ticks and other biting insects may be carriers of an infectious disease. With the advent of global warming, insects and insect-borne infectious diseases are spreading to new areas. To protect yourself against contracting an insect-borne infectious disease, the Centers for Disease Control and Prevention (CDC) recommends using the following insect repellents and insecticides; they have been shown to be safe and effective, even in pregnant and breastfeeding women. Clothing, tents, and mosquito netting are ideal for first order of protection and sleeping, especially when saturated with Permethrin (which kills insects on contact). To protect against chiggers and ticks, wear light-colored or white long pants, long-sleeved shirts, and socks so ticks can be more easily seen; pull socks over pant cuffs. Wear a hat and place petroleum jelly around hairline to keep ticks from crawling into hair (where they will be very difficult to find). Do a thorough tick check each morning & evening before entering and leaving your tent. The CDC does not recommend other insect repellents and products as they have not been shown to be effective despite manufacturers claims. These include natural plant oils, (such as citronella oil, cedar oil, geranium oil (or geraniol), and lemongrass oil), repellents containing vitamin B1 or garlic, and wristbands and ultrasonic devices. Application
DEET
Picaridin
IR3535
Lemon Eucalyptus Oil
Permethrin
Interested in learning first aid? Take one of our wilderness medicine courses. Guides and expedition leaders should consider taking our Wilderness First Responder course.
Looking for a reliable field reference? Consider consider purchasing one of our print or digital handbooks; our digital handbook apps are available in English, Spanish, and Japanese. Updates are free for life. A digital SOAP note app is also available. Pathophysiology Exertional rhabdomyolysis occurs when skeletal muscle breaks down during excessive, repeatitive, and unfamiliar exercise. The severe and unaccustomed exercise stretches the cell membrane, increases its permeability, and leads to the release of myoglobin, creatine kinase, and other harmful proteins into the patient's blood. Severe rhabdomyolysis results in renal failure in 5-7% of cases as myoglobin accumulates in the patient’s blood, spills into their urine, and create deposits (casts) that block the renal tubules and restrict renal blood flow. Death is rare but possible. Dehydration and heat stress exacerbate the condition, especially in unacclimatized individuals. People with Sickle Cell Trait* and those with some metabolic disorders are predisposed to the "rhabdo." Wildland firefighters and those engaging in heavy exercise in similar conditions are at risk, especially during their initial training. *People with Sickle Cell Trait (SCT) inherit the sickle cell gene from one parent and while they do not typically present with the signs and symptoms of Sickle Cell Disease, they are a carrier. Over three million Americans have SCT. Prevention
 Patients with exertional rhabdomyolysis will present with a history of strenuous exercise, often in a moderate to severe heat challenge, severe, often incapacitating muscle pain, and unusually dark urine. In combination, these indicate the need for immediate assessment by a physician. Myoglobin in the urine (myoglobinuria) can be confirmed via a simple urine dipstick test, a positive test indicates testing for high levels of creatine kinase (CK) a muscle enzyme released with myoglobin when skeletal muscle is damaged. CK levels 5-20 times greater than normal are common with exertional rhabdomyolysis. Treatment
Looking for a reliable field reference? Consider consider purchasing one of our print or digital handbooks; our digital handbook apps are available in English, Spanish, and Japanese. Updates are free for life. A digital SOAP note app is also available. Pathophysiology
Allergic anaphylaxis occurs when a patient’s immune system responds inappropriately to a food, drug, or other protein and is mediated by IgE (antibodies); like all allergic reactions, it requires pre-exposure. Common allergens are penicillin or other beta-lactam antibiotics, tree nuts, Hymenoptera venom, and shellfish. But…non-IgE mediated reactions can also occur: Originally known as an anaphylactoid reaction or idiopathic anaphylaxis, triggers act directly on both mast cells and basophils; they are not IgE mediated and do not require pre-exposure. Triggers for non-IgE mediated anaphylaxis include: vancomycin, opiates, aspirin, NSAIDs, temperature, and exercise. Signs, symptoms, and treatment for both IgE mediated and non-IgE mediated anaphylactic reactions is the same. Patient history while useful to avoid triggers, remains somewhat unreliable for predicting future events, especially initial reactions. And, anaphylaxis is on the rise. While epinephrine remains the mainstay of treatment, it is not always successful and fatalities are possible even with treatment. In most cases, anaphylaxis is a mono-phasic reaction: What you see is what you get. That said, roughly 20-30 percent of all anaphylactic reactions are biphasic with the original signs and symptoms returning 3-10+ hours later (rebound). H1 and H2 blockers (antihistamines) and corticosteroids are used to help prevent biphasic reactions, but are not always successful; the available data is inconclusive. Some outdoor programs with long evacuation times carry oral prednisone to be administered under direct physician control—via cell or satellite phone—or by written standing orders Assessment
S/Sx
Treatment
Evacuation
Looking for a reliable field reference? Consider consider purchasing one of our print or digital handbooks; our digital handbook apps are available in English, Spanish, and Japanese. Updates are free for life. A digital SOAP note app is also available.  Cardiopulmonary resuscitation (CPR) and cardiocerebrial resuscitation (CCR) are valuable first aid skills and we should all master them. That said, their effectiveness is severely limited in a wilderness environment. Cardiopulmonary resuscitation uses a combination of chest compressions and rescue breathing to delay brain death and extend the resuscitation window while cardiocerebral resuscitation utilizes chest compressions only; both are potentially life-saving techniques. It takes approximately 10-12 chest compressions to build enough intrathoracic pressure to start circulating blood. The same intrathoracic pressure that circulates the patient’s blood also brings in a small amount of fresh air and oxygen. If there is residual air and oxygen in the lungs—as occurs in cardiac arrest caused by a heart attack—chest compressions alone are more effective in delaying the onset of brain death than when combined with rescue breathing because they maintain a consistent intrathoracic pressure. Conversely, a combination of chest compressions and rescue breathing (CPR) is more effective than CCR for patients whose arrest stems from a primary respiratory problem and lack of available oxygen as occurs in near drowning, lightning, complete snow burial, etc. The effect of both techniques decreases rapidly over time and cannot save or prolong the life of a pulseless patient for greater than 20 minutes and neither CPR or CCR work with major trauma patients whose arrest stems from increased ICP, significant lung damage, or volume shock. For CPR or CCR to be effective the patient’s circulatory system must be intact and their core temperature above 90º F (32º C); your chest compressions must be hard and fast (ideally at least 100 per minute) and delivered in the lower third of the patient’s sternum; your weight must be directly over the patient and the patient’s chest must be allowed to fully recoil between compressions; the recoil is as important as the compression. If rescue breathing is indicated, ventilate until the patient’s chest begins to rise; do not over-inflate—over-inflation forces air into the patient’s stomach and increases the chance or frequency of vomiting. In settings where rapid defibrillation, advanced cardiac life support, and rapid transport to a major hospital are not possible, the overwhelming majority of patients in cardiac arrest will die. It is important that all rescuers understand the limits of CPR and CCR and when it is appropriate to start and stop. When teaching chest compressions in our wilderness medicine courses we often tell students to compress at the rate of the beat in the Bee Gee's disco tune "Staying Alive" or Queen's "Another One Bites the Dust" depending on whether a student views the glass as half full or half empty.... (Yes, humor is important in the medical field.) Looking for a reliable field reference? Consider consider purchasing one of our print or digital handbooks; our digital handbook apps are available in English, Spanish, and Japanese. Updates are free for life. A digital SOAP note app is also available. Okay, winter IS cold. That's why we call it winter. Cold injuries—hypothermia, frostnip, frostbite, chilblains—are all potential problems. Fortunately with a bit of thought and practice, it's possible to stay warm, even in extreme cold. If you are a seasoned winter traveler, you're probably familiar with everything listed here. If you are new to playing outside in the winter, I trust you'll find a few things of value.
Thermoregulation & Cold PhysiologyHypothermia occurs when a person cannot maintain their normal body temperature in the face of a cold challenge. The cold challenge increases as a person is exposed to progressively decreasing temperature, increasing humidity, and increasing wind. People respond to a cold challenge by increasing their heat production through shivering and maintaining their core temperature through peripheral vasoconstriction. Heat production requires an efficient metabolism and accessible calories. The ability to produce heat via shivering or exercise drops as their available calories become depleted. Fitness, hydration, health, and injury all affect a person’s metabolism and their ability to produce heat.
The onset of hypothermia is variable and depends on the severity of the cold challenge, the length of exposure, and the health of the patient. Acute hypothermia may occur in minutes to hours with cold water immersion regardless of the victim’s health. Subacute hypothermia may occur in hours to days in a mountain or river environment where decreased calories predispose the climber, hiker, or paddler to hypothermia from a moderate cold challenge. Expedition members with predisposing factors (poor health, inadequate nutrition, poor hydration, etc.) can develop a chronic cold response during prolonged exposure (days to weeks) to cool environmental conditions due to limited caloric intake and no glycogen or fat stores. They may easily become hypothermic when presented with a slight increase in the cold challenge. Boaters go out in all kinds of weather. Each year numerous people die by falling into cold water or capsizing their small boats; some die quickly due to drowning, others more slowly from hypothermia. Some are on their own trips; others on guided trips. All are typically unprepared. Pathophysiology Water cools the body 25-30 times faster than air. Cooling occurs faster if the water is moving, as happens when a victim is immersed in current, whitewater, or waves, and even faster if the victim is swimming or struggling. Photo 1 shows heat loss from a body in the air; photo 2 shows heat loss from the core when an immersion victim remains motionless in cold water; photo 3 shows heat loss from the extremities while swimming cold water. Muscle tissue produces heat even at rest; during heavy exercise heat production increases more than ten-fold. The more insulation—clothing and/or fat—a victim has, the slower they cool. The rate of cooling is also proportional the victim's surface to mass ratio. Large, fat people cool significantly slower than small, thin people; adults cool slower than children. |
Categories
All
Our public YouTube channel has educational and reference videos for many of the skills taught during our courses. Check it out!
|



 RSS Feed
RSS Feed
