|
Deaths due to opioid overdoses continue to rise. Opioid abuse knows no age, race, or economic barriers; and, abuse is often hidden, making it difficult to know who is at risk for an overdose. In April 2018 U.S. Surgeon General, Dr. Jerome Adams, issued a public health advisory urging more Americans to learn to use and carry naloxone. Most states have approved Narcan® Nasal Spray for over the counter sales and publicly encourage addicts, family, and friends to carry it. Communities provide training and naloxone to police and place naloxone in public places with AEDs; some public health agencies provide it for free. Colleges and universities provide training and naloxone to staff and students. While still uncommon, opioid overdoses have occurred in wilderness settings. This begs the following questions:
What are Opioids? Heroin, morphine, codeine, and thebaine are naturally occurring opioids made from the resin of poppy plants; hydromorphone, hydrocodone, and oxycodone are derived from resin in a lab setting. Fentanyl, pethidine, levorphanol, methadone, tramadol, and dextropropoxyphene are synthetic. All opioids depress the central nervous system (CNS) and cause feelings of euphoria; when used correctly, for short periods of time, they are effective pain medicines. All are physiologically addictive. Chronic opioid users develop a tolerance for the drug and require increasingly higher doses to achieve the same level of pain control or well-being. (Note: Opioids are often mixed with other drugs for recreational purposes.) Withdrawal signs and symptoms are the result of excessive stimulus of the sympathetic nervous system and include: increased pulse rate and blood pressure, restlessness, tremors, sleeplessness, muscle and bone pain, abdominal pain, diarrhea, vomiting, sweating, and shivering; patients in acute withdrawal may become combative. As opioid tolerance increases so does dependence…and the severity of withdrawal S/Sx. An opioid overdose typically occurs when someone takes a large amount of an opioid or a drug containing an opioid, mixes opioids with alcohol, or had a recent change in their level of tolerance. Life-threatening signs and symptoms of an opioid overdose include:
What is Naloxone? Naloxone is an opioid antagonist; it binds with and blocks opioid receptor sites in the brain, reversing the signs and symptoms of an overdose. In order to be effective, naloxone must be given before the patient goes into cardiac arrest. Except in extremely rare cases when someone is allergic to naloxone, administering naloxone to a patient who is not suffering from an oipoid overdoese does no harm. Naloxone will not prevent deaths caused by other drugs: alcohol, speed, cocaine, or sedatives (e.g.: benzodiazepines like Xananx®, Valium®, etc.). While there are numerous delivery methods only two are conducive to using in a remote setting: intranasal spray and intramuscular (IM) or subcutaneous (SQ) injection. Of the two, only Narcon® nasal spray is available over the counter in most states, making the choice easy for lay people, outdoor educators, and guides. Naloxone delivered as a nasal spray or injection takes roughly 3-5 minutes to act. If there is no response after five minutes, give another dose. Naloxone is metabolized in the liver within 30-90 minutes and its metabolites excreted in the urine over the next 3-4 days. Because naloxone is metabolized faster than most opioids—especially long-acting opioids like methadone or sustained-release pain compounds—it’s vital to carry more than one dose. Patients should be monitored for 2-3 hours as further doses may be necessary to treat a relapse. Acute withdrawal symptoms are possible but rare with intranasal administration of naloxone but cause for concern should they occur as the the patient may become combative and a danger to themselves and others. Naloxone slowly loses its potency over time or if it is exposed to too much heat, cold, or sunlight. That said, using expired naloxone will not cause harm but you may need more doses to reverse the S/Sx of an opioid overdose. Ideally you should replace expired all expired drugs, and store naloxone in a dark and dry place between 80°F (25°C) and 40°F (5°C)...you want to make sure that it is easily accessible should you need it. When should I administer naloxone?
 Directions for administering an intramuscular injection of naloxone Carry naloxone in a 1 ml snap-top vial (they are easier to use than a 1 ml ampoule); dose is 0.4 mg/ml. Consider carry a vial and syringe in a capped PVC pipe container; use the capped pipe as a sharps container to safely carry the used needle and syringe out of the backcountry for disposal. Use a 21 to 23 gauge needle 1 to 1.5 inches long for an adult.
Interested in learning more about wilderness medicine? Take one of our wilderness medicine courses. Guides and expedition leaders should consider taking our Wilderness First Responder course.
Looking for a reliable field reference? Consider consider purchasing one of our print or digital handbooks; our digital handbook apps are available in English, Spanish, and Japanese. Updates are free for life. A digital SOAP note app is also available.
0 Comments
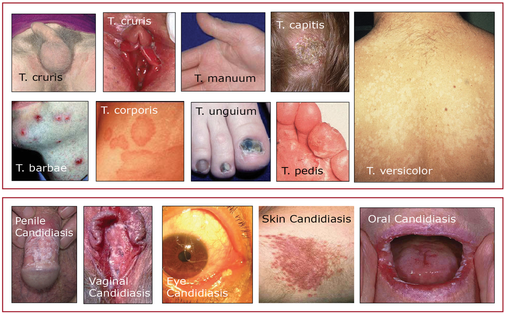
Pathophysiology Numerous types of fungi live on and in our bodies without causing harm; they are held in check by competing bacteria and our immune system. Disease-causing fungi can be divided into two groups: filamentous fungi and yeasts. Filamentous fungi are made up of branching threads known as hyphae; yeasts are single-celled organisms. The most common fungal infections are superficial and caused by Tinea, a filamentous fungi and Candida albicans, a yeast. Heat, humidity, immunocompromised states, long term antibiotic use, diabetes, and steroid therapy predispose people to both types of fungal infections. Fungal infections are more common in the summer and exerted by wearing synthetic clothing and sweating. Tinia Infections Tinea infections are caused by a group of fungi (ringworm) that live on keratinous structures and invade dead layers of the host's skin, hair, and nails; the transmission routes are direct contact with an infected person or animal or with contaminated soil. Clinically, tinea infections are classified according to the body region involved/infected: tinea capitis (scalp), tinea corporis and versicolor (trunk and extremities), tinea manuum and tinea pedis (palms, soles, and interdigital webs), tinea cruris (groin), tinea barbae (beard area and neck), tinea faciale (face), and tinea unguium (nails). Candida Albicans (Yeast) Infections Candida albicans skin infections may closely mimic tinea crurisare but are usually moister, more inflammatory, and associated with satellite macules, pustules, and scales. Unlike Tinea, Candida may also infect the mucus membranes of the mouth, vagina, penis, and eye. These infections are red, itchy, moist and often associated with a yeasty odor and a white cheese-like discharge. Most mucosal infections result from long-term antibiotic use. Prevention
Assessment
Treatment
Don't know where to begin or what to do? Take one of our wilderness medicine courses. Guides and expedition leaders should consider taking our Wilderness First Responder course.
Looking for a reliable field reference? Consider consider purchasing one of our print or digital handbooks; our digital handbook apps are available in English, Spanish, and Japanese. Updates are free for life. A digital SOAP note app is also available. Pathophysiology Exertional rhabdomyolysis occurs when skeletal muscle breaks down during excessive, repeatitive, and unfamiliar exercise. The severe and unaccustomed exercise stretches the cell membrane, increases its permeability, and leads to the release of myoglobin, creatine kinase, and other harmful proteins into the patient's blood. Severe rhabdomyolysis results in renal failure in 5-7% of cases as myoglobin accumulates in the patient’s blood, spills into their urine, and create deposits (casts) that block the renal tubules and restrict renal blood flow. Death is rare but possible. Dehydration and heat stress exacerbate the condition, especially in unacclimatized individuals. People with Sickle Cell Trait* and those with some metabolic disorders are predisposed to the "rhabdo." Wildland firefighters and those engaging in heavy exercise in similar conditions are at risk, especially during their initial training. *People with Sickle Cell Trait (SCT) inherit the sickle cell gene from one parent and while they do not typically present with the signs and symptoms of Sickle Cell Disease, they are a carrier. Over three million Americans have SCT. Prevention
 Patients with exertional rhabdomyolysis will present with a history of strenuous exercise, often in a moderate to severe heat challenge, severe, often incapacitating muscle pain, and unusually dark urine. In combination, these indicate the need for immediate assessment by a physician. Myoglobin in the urine (myoglobinuria) can be confirmed via a simple urine dipstick test, a positive test indicates testing for high levels of creatine kinase (CK) a muscle enzyme released with myoglobin when skeletal muscle is damaged. CK levels 5-20 times greater than normal are common with exertional rhabdomyolysis. Treatment
Looking for a reliable field reference? Consider consider purchasing one of our print or digital handbooks; our digital handbook apps are available in English, Spanish, and Japanese. Updates are free for life. A digital SOAP note app is also available. Pathophysiology
Allergic anaphylaxis occurs when a patient’s immune system responds inappropriately to a food, drug, or other protein and is mediated by IgE (antibodies); like all allergic reactions, it requires pre-exposure. Common allergens are penicillin or other beta-lactam antibiotics, tree nuts, Hymenoptera venom, and shellfish. But…non-IgE mediated reactions can also occur: Originally known as an anaphylactoid reaction or idiopathic anaphylaxis, triggers act directly on both mast cells and basophils; they are not IgE mediated and do not require pre-exposure. Triggers for non-IgE mediated anaphylaxis include: vancomycin, opiates, aspirin, NSAIDs, temperature, and exercise. Signs, symptoms, and treatment for both IgE mediated and non-IgE mediated anaphylactic reactions is the same. Patient history while useful to avoid triggers, remains somewhat unreliable for predicting future events, especially initial reactions. And, anaphylaxis is on the rise. While epinephrine remains the mainstay of treatment, it is not always successful and fatalities are possible even with treatment. In most cases, anaphylaxis is a mono-phasic reaction: What you see is what you get. That said, roughly 20-30 percent of all anaphylactic reactions are biphasic with the original signs and symptoms returning 3-10+ hours later (rebound). H1 and H2 blockers (antihistamines) and corticosteroids are used to help prevent biphasic reactions, but are not always successful; the available data is inconclusive. Some outdoor programs with long evacuation times carry oral prednisone to be administered under direct physician control—via cell or satellite phone—or by written standing orders Assessment
S/Sx
Treatment
Evacuation
Looking for a reliable field reference? Consider consider purchasing one of our print or digital handbooks; our digital handbook apps are available in English, Spanish, and Japanese. Updates are free for life. A digital SOAP note app is also available.  Cardiopulmonary resuscitation (CPR) and cardiocerebrial resuscitation (CCR) are valuable first aid skills and we should all master them. That said, their effectiveness is severely limited in a wilderness environment. Cardiopulmonary resuscitation uses a combination of chest compressions and rescue breathing to delay brain death and extend the resuscitation window while cardiocerebral resuscitation utilizes chest compressions only; both are potentially life-saving techniques. It takes approximately 10-12 chest compressions to build enough intrathoracic pressure to start circulating blood. The same intrathoracic pressure that circulates the patient’s blood also brings in a small amount of fresh air and oxygen. If there is residual air and oxygen in the lungs—as occurs in cardiac arrest caused by a heart attack—chest compressions alone are more effective in delaying the onset of brain death than when combined with rescue breathing because they maintain a consistent intrathoracic pressure. Conversely, a combination of chest compressions and rescue breathing (CPR) is more effective than CCR for patients whose arrest stems from a primary respiratory problem and lack of available oxygen as occurs in near drowning, lightning, complete snow burial, etc. The effect of both techniques decreases rapidly over time and cannot save or prolong the life of a pulseless patient for greater than 20 minutes and neither CPR or CCR work with major trauma patients whose arrest stems from increased ICP, significant lung damage, or volume shock. For CPR or CCR to be effective the patient’s circulatory system must be intact and their core temperature above 90º F (32º C); your chest compressions must be hard and fast (ideally at least 100 per minute) and delivered in the lower third of the patient’s sternum; your weight must be directly over the patient and the patient’s chest must be allowed to fully recoil between compressions; the recoil is as important as the compression. If rescue breathing is indicated, ventilate until the patient’s chest begins to rise; do not over-inflate—over-inflation forces air into the patient’s stomach and increases the chance or frequency of vomiting. In settings where rapid defibrillation, advanced cardiac life support, and rapid transport to a major hospital are not possible, the overwhelming majority of patients in cardiac arrest will die. It is important that all rescuers understand the limits of CPR and CCR and when it is appropriate to start and stop. When teaching chest compressions in our wilderness medicine courses we often tell students to compress at the rate of the beat in the Bee Gee's disco tune "Staying Alive" or Queen's "Another One Bites the Dust" depending on whether a student views the glass as half full or half empty.... (Yes, humor is important in the medical field.) Looking for a reliable field reference? Consider consider purchasing one of our print or digital handbooks; our digital handbook apps are available in English, Spanish, and Japanese. Updates are free for life. A digital SOAP note app is also available. Over the counter (OTC) acetaminophen, ibuprofen, and naproxen are commonly used to treat pain and fever. Because they are labeled and packaged for OTC use most people consider them safe. This is not true. In addition, many people also believe that more is better. This is also not true. In fact all three medications have the potential for serious side effects. Aging further increases the risk of serious side effects as older people, especially those over the age of 65, often have a decrease in liver and kidney function and are mildly dehydrated.
In addition to its therapeutic effects, acetaminophen is a dose-dependent liver toxin; patient who take acetaminophen with alcohol or while fasting-due to illness, anorexia, or malnutrition-are at serious risk for liver failure. Even if taken at the current OTC recommended dose (not to exceed 4 g/day), the drug can be toxic. The FDA expert panel recommends lowering the standard dose from 1,000 mg to 650 mg and the maximum dose/day to 3 g/day. Accidental overdose send roughly 80,000 people to the emergency department each year; at least 500 are fatal. Part of the problem is that acetaminophen is found in more than 600 OTC medications including cold, flu, sinus, and in Rx codeine-based medications (Vicodin® or Percocet®). Patients unaware of the potential for serious complications often mix and match drugs containing acetaminophen and easily exceed the maximum daily dose. Forewarned is forearmed. Ibuprofen and naproxen also have serious side effects. Chronic use of both, including aspirin, may cause indigestion, gastric or duodenal ulcers, and fluid retention. In addition, ibuprofen use slightly increases the risk of a heart attack or stroke. Renal damage is also possible and significantly increases if the patient is dehydrated (as is often the case in an outdoor setting). Not surprisingly the risk of adverse effects increases substantially with dose and course. Note that while many athletes take ibuprofen or naproxen for general muscle soreness, neither drug has been shown to be effective. Remember that the GI side effects of both drugs increase if the drug is not taken with food and the renal effects increase if the patient or athlete is dehydrated. Follow the following simple guidelines greatly reduces your chance of adverse effects:
Interested in learning first aid? Take one of our wilderness medicine courses. Guides and expedition leaders should consider taking our Wilderness First Responder course. Looking for a reliable field reference? Consider consider purchasing one of our print or digital handbooks; our digital handbook apps are available in English, Spanish, and Japanese. Updates are free for life. A digital SOAP note app is also available. Have you ever experienced sudden sharp chest pain that lasts for up to a minute before disappearing and leaving a soreness—or an awareness of pain—that gradually disappears over the next few minutes? Did it appear on the left side of your chest below your left nipple? Was it so intense you didn't want to breathe or move? Did you think you, for a split second, "OMG, I'm too young to have a heart attack?" If so, you are one of many. Not to worry, the pain has nothing to do with your heart despite it's proximity and, while its exact cause remains unknown, it's probably due to a pinched nerve. In fact, the condition is so common, it's medically known as Precordial Catch Syndrome (PCS). It occurs more often in children and teenagers but can persist into adulthood. Some people report the sensation of a bubble popping immediate before the pain recedes. There are no apparent triggers; PCS can occur during exercise or rest and may present multiple times in one day or at irregular times over multiple years.
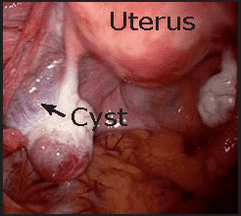 Pathophysiology Most Ovarian Cysts are small fluid-filled sacs that develop in a woman's ovaries as a normal part of a women’s menstrual cycle. During childbearing years a women produces a single egg once a month in a small sac called a follicle. The release of estrogen signals the sac to rupture and release the egg into the fallopian tube where it travels to the uterus. If the egg is fertilized, it implants on the uterine wall; unfertilized eggs are expelled with the uterine lining during menstruation. If the follicle fails to rupture and release the egg, fluid remains in the sac and a follicular cyst may form. Another type of cyst (corpus luteum cyst) can form even if the egg is released; this type of cyst contains a small amount of blood. Small cysts of either type—less than one half an inch—are common, produce no symptoms, and disappear on their own in a few weeks. A large cyst may cause pressure, bloating, pelvic pain, pain during intercourse if bumped, a increased desire to urinate, or a late period. Sudden and severe pelvic pain, often accompanied by nausea and vomiting, may be a sign of twisting of the ovary and reducing its blood supply or the rupture of a cyst and internal bleeding. If benign, the pain will improve dramatically within 45 minutes.
Developing atherosclerosis, plaque rupture, and subsequent clotting of a coronary artery is the most common cause of heart attacks. Signs and symptoms commonly appear immediately and are due to a lack of oxygen in the affected tissue. Cardiac arrest is unpredictable and if it occurs is ultimately due to a change in the electrical impulses and conduction pattern in the specialized cardiac nerves that stimulate normal cardiac contractions. An injury to these nerves blocks the conduction pathway. The block prevents or delays the electrical impulses from reaching their destination and causes cardiac arrest. The potential for arrest from a heart attack is directly related to the type, location, and size of the compromised tissue. If the blocked artery services the specialized conduction cells that coordinate the pumping action of the heart, arrest occurs within seconds or minutes. If the blocked artery services the heart’s contractile fibers rather than its specialized conduction cells, the pumping action of the heart may be compromised. A reduction in the heart’s ability to pump blood efficiently may cause a back pressure in the pulmonary vessels and force fluid into the alveoli causing respiratory distress, fatigue, swelling in the hands and feet, indigestion and loss of appetite. Complete pump failure and arrest may develop if a significant amount of heart muscle has been injured and the heart cannot continue to meet the body’s demands for nutrients. Emergency aspirin therapy increases the chance of survival, minimizes permanent damage, and improves recovery. The longer arrest is delayed the more likely the patient will survive without immediate hospital treatment.
|
Categories
All
Our public YouTube channel has educational and reference videos for many of the skills taught during our courses. Check it out!
|


 RSS Feed
RSS Feed
