|
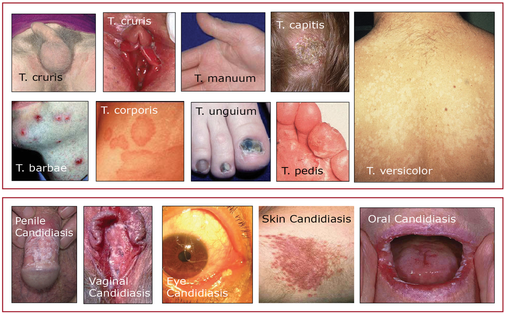
Pathophysiology Numerous types of fungi live on and in our bodies without causing harm; they are held in check by competing bacteria and our immune system. Disease-causing fungi can be divided into two groups: filamentous fungi and yeasts. Filamentous fungi are made up of branching threads known as hyphae; yeasts are single-celled organisms. The most common fungal infections are superficial and caused by Tinea, a filamentous fungi and Candida albicans, a yeast. Heat, humidity, immunocompromised states, long term antibiotic use, diabetes, and steroid therapy predispose people to both types of fungal infections. Fungal infections are more common in the summer and exerted by wearing synthetic clothing and sweating. Tinia Infections Tinea infections are caused by a group of fungi (ringworm) that live on keratinous structures and invade dead layers of the host's skin, hair, and nails; the transmission routes are direct contact with an infected person or animal or with contaminated soil. Clinically, tinea infections are classified according to the body region involved/infected: tinea capitis (scalp), tinea corporis and versicolor (trunk and extremities), tinea manuum and tinea pedis (palms, soles, and interdigital webs), tinea cruris (groin), tinea barbae (beard area and neck), tinea faciale (face), and tinea unguium (nails). Candida Albicans (Yeast) Infections Candida albicans skin infections may closely mimic tinea crurisare but are usually moister, more inflammatory, and associated with satellite macules, pustules, and scales. Unlike Tinea, Candida may also infect the mucus membranes of the mouth, vagina, penis, and eye. These infections are red, itchy, moist and often associated with a yeasty odor and a white cheese-like discharge. Most mucosal infections result from long-term antibiotic use. Prevention
Assessment
Treatment
Don't know where to begin or what to do? Take one of our wilderness medicine courses. Guides and expedition leaders should consider taking our Wilderness First Responder course.
Looking for a reliable field reference? Consider consider purchasing one of our print or digital handbooks; our digital handbook apps are available in English, Spanish, and Japanese. Updates are free for life. A digital SOAP note app is also available.
2 Comments
lorrenaine peltier
11/15/2018 12:35:25 am
Diagnosis, treatment, and prevention
Reply
Your comment will be posted after it is approved.
Leave a Reply. |
Categories
All
Our public YouTube channel has educational and reference videos for many of the skills taught during our courses. Check it out!
|
 RSS Feed
RSS Feed
