 Click image to enlarge. Click image to enlarge. General Assessment & Treatment Strategies for Medical Problems
Red Flags for Urgent Medical Evacuations
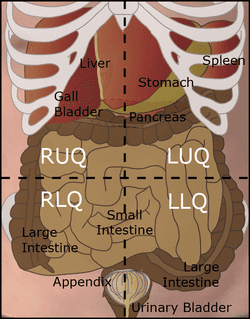
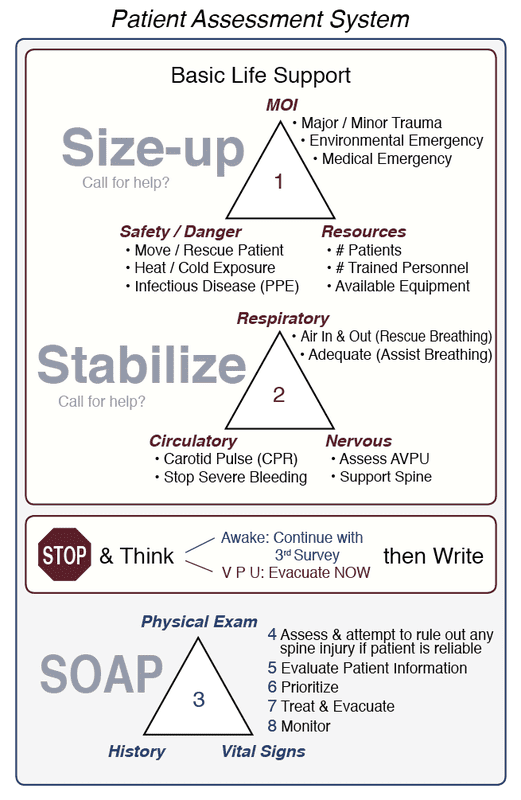
The urgency of an evacuation depends on the degree of involvement, or potential involvement, of any critical system. The greater the degree or potential, the more urgent the evacuation. If possible, consult with a physician. When in doubt, take them out. Diagnostic patterns for a non-urgent Level 3 Evacuation and red flags for an urgent Level 2 or Level 1 Evacuation are discussed below. Level 3 Evacuation
Level 2 Evacuation
Level 1 Evacuation
Want more information on this and other wilderness medicine topics? Take one of our wilderness medicine courses. Guides and expedition leaders should consider taking our Wilderness First Responder course. Looking for a reliable field reference? Consider consider purchasing one of our print or digital handbooks; our digital handbook apps are available in English, Spanish, and Japanese. Updates are free for life. A digital SOAP note app is also available.
0 Comments
Your comment will be posted after it is approved.
Leave a Reply. |
Categories
All
Our public YouTube channel has educational and reference videos for many of the skills taught during our courses. Check it out!
|
 RSS Feed
RSS Feed
