|
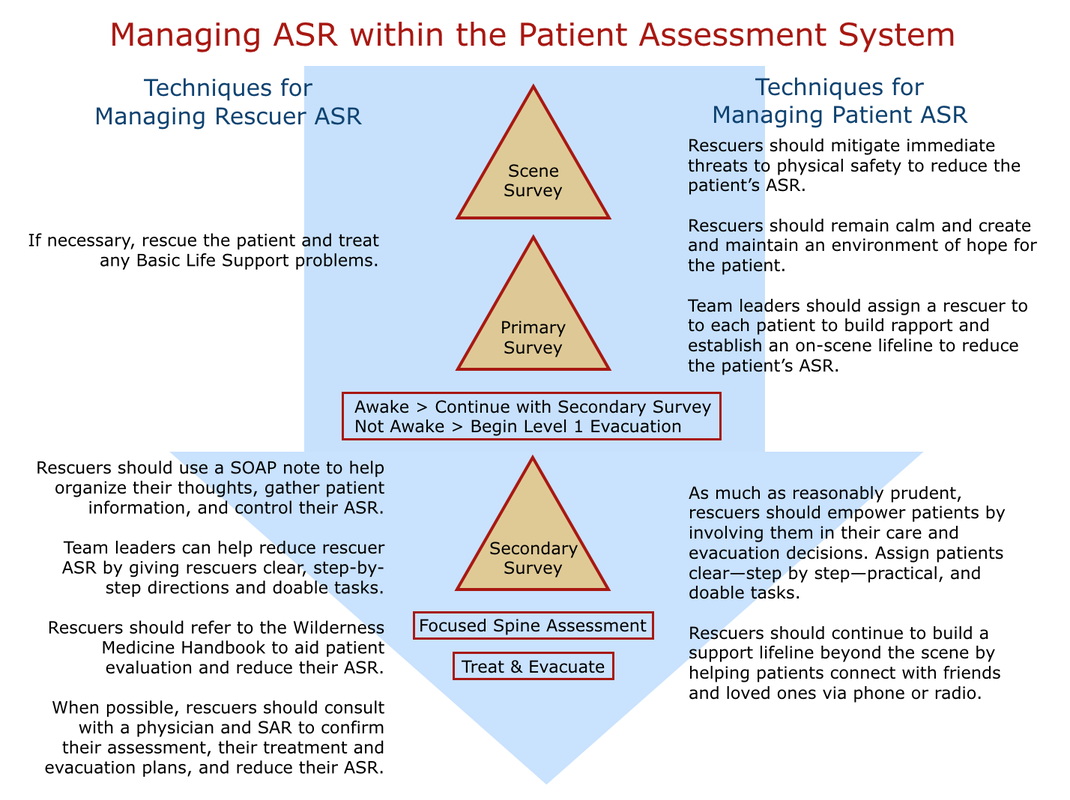
On a functional level, the nervous system is divided into two divisions: the voluntary (somatic) nervous system and the involuntary (autonomic) nervous system. The voluntary division of the nervous system contains both sensory and motor nerves. Sensory nerves carry input to the spinal cord and brain, while motor nerves carry messages from them. Through its nerves, the somatic nervous system controls conscious functions, principally high-level thought and striated muscle contractions. The autonomic division maintains or restores homeostasis by regulating smooth muscle contractions and the glandular secretion of hormones. Most autonomic functions are beyond conscious control. The autonomic division of the nervous system is subdivided into the sympathetic and the parasympathetic systems. The sympathetic system stimulates effectors (cells or organs) while the parasympathetic system inhibits them. Both systems continually transmit impulses to the same effector and act in an antagonistic manner, with the stronger impulse assuming control. Under normal conditions, the sympathetic system is responsible for waking us up and the parasympathetic system is responsible for sleep and digestion. If the sympathetic nervous system is engaged during a stress response, the body prepares for “fight or flight”: pupils dilate to increase vision; pulse, respiration and blood pressure rates rise to meet an intense physical demand; awareness, often seen as anxiety, increases; sweating increases, while vasoconstriction leaves the skin pale, cool and moist; and endorphins are released to block pain. Over stimulation of muscle fibers often results in uncontrollable shaking. A strong sympathetic response decreases cognitive function leaving patients unable to process complex information and feeling overwhelmed and often fearful. A patient experiencing a sympathetic ASR cannot give accurate information about their injuries. In most cases, they are unaware of any physical injuries and may not exhibit abnormal signs or symptoms upon examination. Their vital sign pattern may mimic or mask volume shock. If the parasympathetic nervous system is stimulated, the patient becomes nauseated, dizzy, and may faint. Blood pools centrally around their digestive tract and their pulse, respiratory and blood pressure rates fall. Their skin is pale and cool. Upon awakening, the patient is often confused. A parasympathetic ASR may mimic the signs and symptoms of a concussion and make accurate assessment of a traumatic head injury difficult. A serious medical incident is often stressful to all involved: rescuers, care providers, patients, and bystanders; and, any or all involved may have both immediate and lingering effects: Post Traumatic Stress Disorders (PTSD) are common, although individual reactions vary considerably. Your actions as a rescuer or care provider can mitigate your patient's stress in both the short term and long term. And as a scene leader, the same strategies apply to working with expedition members or your rescue team and bystanders. The term "Psychological First Aid (PFA)" has been used in recent years to identify strategies that have proven to help prevent or reduce both the short (ASR) and long term (PTSD) effects of stress. While the term may be new, the strategies discussed below should not be: Psychological First Aid is—and has been—an intentional and integral part of our Patient Assessment System. The strategies below align with current PFA principles. As much as possible, rescuers should strive to create as safe an environment as possible in the aftermath of an overwhelming event by mitigating scene threats and calming patients, bystanders, and rescuers as necessary. It's vital not to lie to patients, bystanders, or team members but to be realistic and focus on what you—and they—can do, and are doing to keep them safe. This may include removing select people from the scene or shielding them from a chaotic scene. Remember that stress affects everyone, including rescuers and care providers. You must first reduce your sympathetic ASR (fight or flight response) before attempting to help others. Again, be truthful and focus on the present. As much as possible, radiate calm. Following the Patient Assessment System and using SOAP notes help caregivers reduce their ASR by providing an organized, step by step thought process, that also acts to calm their patients. It's easy for both patients and rescuers to feel powerless or helpless in what they perceive as extreme situations where no clear avenue forward is visible. Care providers can empower patients by involving them in their care and evacuation decisions where appropriate, and where appropriate in the care of others. And team leaders can empower rescuers, care providers, and bystanders by assigning clear—step by step—practical, and doable tasks. Team leaders can also build an on-scene support network by assigning a care provider to each patient and have them remain with the patient throughout their assessment, treatment, and evacuation (they do not have to be the primary care provider). The relationship between a care provider and patient provides a very real lifeline for severely stressed patients. Both team leaders and care providers can also work to extend the support lifeline beyond the scene by helping patients and bystanders connect with their friends, family, and pets as soon as possible. ln combination with shared, relevant stories, all of the above combine to help inspire hope for the current situation. Looking for a reliable field reference? Consider consider purchasing one of our print or digital handbooks; our digital handbook apps are available in English, Spanish, and Japanese. Updates are free for life. A digital SOAP note app is also available.
0 Comments
Your comment will be posted after it is approved.
Leave a Reply. |
Categories
All
Our public YouTube channel has educational and reference videos for many of the skills taught during our courses. Check it out!
|
 RSS Feed
RSS Feed
