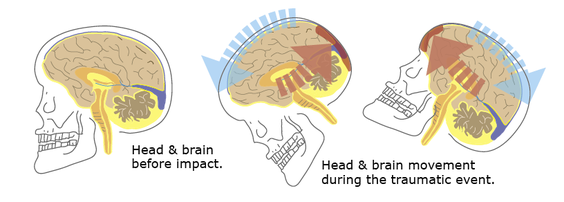
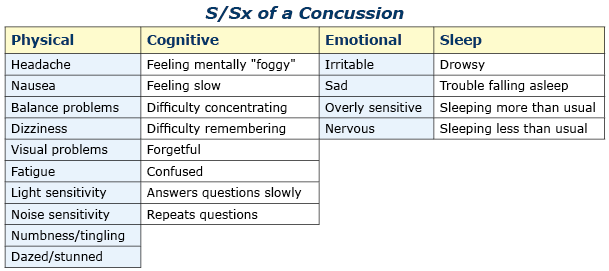
PathophysiologyThe mechanism of injury (MOI) is a direct blow to the patient’s head or a direct blow to another part of their body where the force is transmitted to their brain via their spinal column, cord, and associated soft tissue (aka: whiplash). The brain essentially floats inside the skull in cerebral spinal fluid (CFS). The fluid acts to protect and cushion sensitive brain tissue from minor impacts in much the same way as egg white protects the yolk. If the force generated by the traumatic event is strong enough, the brain will bounce off inside of the skull damaging sensitive brain tissue (as shown in the illustrations below). A concussive injury, should it occur, can be functional or structural. A person with a functional concussive injury will present or develop S/Sx, typically within two hours; however, standard imaging techniques (CT, MRI) show no structural damage. The S/Sx of a functional injury—see the chart below—are likely caused by axional stretching and disruption of ion channels, follow a predefined progression, and usually resolve on their own within 7-10 days; although, in some cases, S/Sx may persist for months. That said, structural damage is possible and may lead to increased intracranial pressure (ICP) and potentially death in rare cases. The concern from a field perspective is whether a person with an apparent positive MOI can remain in the field or requires an evacuation. And, if an evacuation is necessary: What is its urgency? Emergency department physicians typically rely on one of seven clinical algorithms to decide if a patient requires imaging or not (Click here to read an article that discusses the pros and cons of each rule), only the High Risk Criteria for the Canadian CT Head Injury Rule and the NEXUS II can be easily extrapolated to aid evacuation decisions in the field; both may be used in the presence of a significant mechanism of injury. It's important to remember that the guidelines are conservative and few concussed patients go on to develop increased ICP. Assessment All people with a positive mechanism must be evaluated for a potential traumatic brain injury (TBI). TBIs can be grossly subdivided into concussion and increased ICP. Concussions can be further subdivided into mild, moderate, and severe, while increased ICP can be broken down into early and late. After a traumatic MOI a patient may present with any of the problems discussed below and progress, or not, from that point. Note that the problems are mutually exclusive and a patient may only have one problem—concussion or increased ICP—at any given time. Seizures are possible at any point especially in infants and young children and common in unresponsive patients with late increased ICP prior to posturing. Patient's with serious head injuries typically have obvious soft tissue damage to their head including:
Mild Concussion
Moderate Concussion
Severe Concussion The distinction between a moderate and severe concussion is important as the mechanism MAY have been severe enough to structurally injure brain cells or small blood vessels, cause intracranial leaks and swelling, and lead to increased ICP. Worsening S/Sx over the next 24 hours indicate a more severe injury (severe concussion) and can be difficult to recognize if the patient is not closely monitored. Pay close attention to the patient’s overall function: Are their S/Sx severe enough that they interfere with their daily function (severe concussion)? When doubt, choose the worst reasonable case scenario.
Early Increased ICP
Late Increased ICP
Treatment Mild Concussion
Moderate Concussion
Severe Concussion
Early Increased ICP
Late Increased ICP
Looking for a reliable field reference? Consider consider purchasing one of our print or digital handbooks; our digital handbook apps are available in English, Spanish, and Japanese. Updates are free for life. A digital SOAP note app is also available.
0 Comments
Your comment will be posted after it is approved.
Leave a Reply. |
Categories
All
Our public YouTube channel has educational and reference videos for many of the skills taught during our courses. Check it out!
|


 RSS Feed
RSS Feed
