IntroductionThe Act of Drowning Contrary to how it is often depicted in movies, the act of drowning often goes unnoticed. There appear to be three separate actions or body positions people adopt when confronted with the possibility of drowning. Depending on their swimming ability, injuries, or illnesses, some will progress through all three of these stages, while others will not.
Drowning In drowning, the victim is submerged under or immersed in water and requires rescue or assistance; not all drowning victims are unresponsive during their rescue; they may be awake, voice responsive, or pain responsive. Drowning is a process with three possible outcomes:
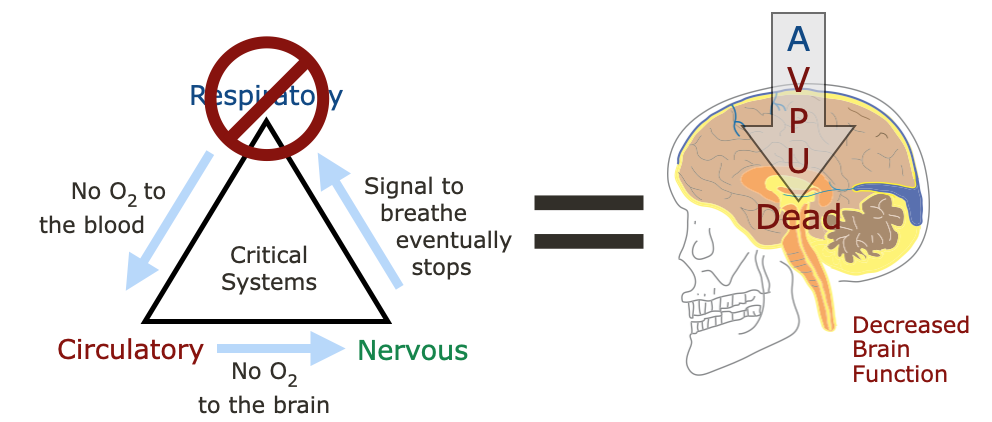
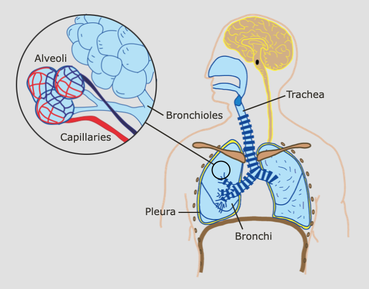
Ultimately, drowning patients die from a lack of oxygen. Our lungs cannot extract oxygen from water. Anatomy & Physiology
Pathophysiology Contrary to popular belief, very little water enters the lungs of most drowning victims:
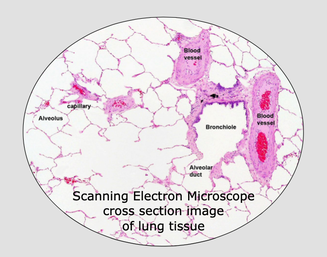
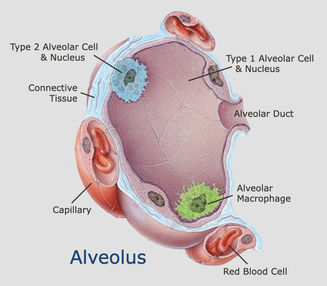
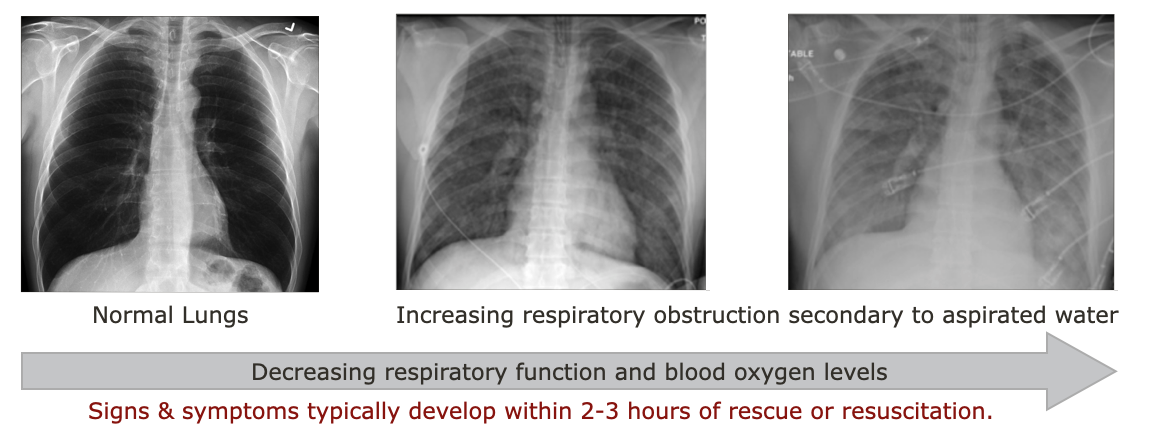
Why so little? When water enters the drowning victim's mouth and nose, their epiglottis immediately closes and covers the trachea and they reflexively swallow. As a result, literally liters of water has been found in the stomachs of fatal drowning victims. This reflexive protection typically remains intact until the patient becomes runs out of oxygen and gasps for air or becomes unresponsive, and even then, little water actually enters the victim's lungs. Unfortunately, it doesn't take much aspirated water to cause problems and interfere with the gas exchange in the alveoli. Patients who have a pulse and are breathing after rescue or resuscitation, may develop respiratory complications severe enough to cause death minutes to hours after the incident if they aspirate enough water.
Basic Life Support Assessment & Treatment
Follow up Assessment, Treatment, & Evacuation
Interested in learning more about wilderness medicine? Take one of our wilderness medicine courses. Guides and expedition leaders should consider taking our Wilderness First Responder course.
Looking for a reliable field reference? Consider consider purchasing one of our print or digital handbooks; our digital handbook apps are available in English, Spanish, and Japanese. Updates are free for life. A digital SOAP note app is also available.
0 Comments
Leave a Reply. |
Categories
All
Our public YouTube channel has educational and reference videos for many of the skills taught during our courses. Check it out!
|

 RSS Feed
RSS Feed
